A polyp is an ingrowth of extra tissue which starts off as a small bump in the lining then later grows to look like a mushroom.
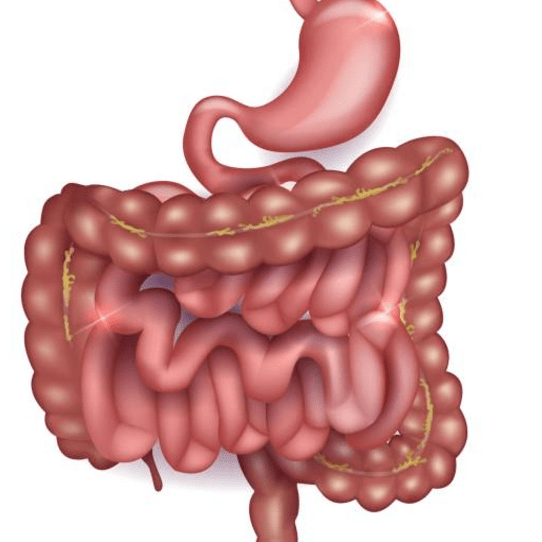
Colonic polyps grow in the large intestine. The large intestine, also called the colon, is a long hollow tube at the end of the digestive tract where ingested food undergoes the final digestive processes to be discharged as faecal material or stools. Colonic polyps are not necessarily dangerous and in fact, most are benign meaning they are not cancerous. But over time, some polyps can develop cancerous cells. Usually, polyps that are smaller than a pea are not harmful. But larger polyps could eventually develop into cancer or may already be cancerous. To be safe, gastroenterologists remove all polyps and test them histologically for the presence of cancerous cells.
Anyone can develop polyps, but certain people are more likely than others. You may have a greater chance of developing polyps if:
- you’re over 50 (The older you are, the more likely you are to develop polyps)
- you’ve had polyps before
- someone in your family has had polyps
- someone in your family has had cancer of the large intestine
You also may be more likely to develop polyps if you:
- eat a lot of fatty foods
- smoke
- drink alcohol
- don’t exercise
- weigh too much
Symptoms
Most small polyps don’t cause symptoms. Often, people don’t know they have one until the doctor finds it during a regular health examination or while testing them for something else.
But some people do have symptoms like these:
- anal bleeding (blood on your underwear or on toilet paper after you’ve had a bowel movement)
- constipation or diarrhoea that lasts more than a week
- blood in the stool (blood can make stool look black, or it can show up as red streaks in the stool)
If you have any of these symptoms, see your doctor to find out what the problem is, as you may need to be referred to a gastroenterologist.
Diagnosis
Gastroenterologists can use a number of tests to check for polyps:
Digital rectal exam. The doctor wears gloves and feels the inner lumen of your rectum for polyps manually.
Barium enema. The doctor places liquid barium in your rectum, before taking an x-ray of your large intestine. Barium, being radio opaque, makes your intestine look white in the x-rays and outlines the polyps as ingrowths from the intestinal wall.
Sigmoidoscopy. This is an older technique but is sometimes used where the doctor can see inside the lower large intestine while the patient is under sedation. The doctor puts a thin flexible tube into the rectum. The device is called an endoscope, which is equipped with a light source, fibre optics and a miniature video camera. Gastroenterologists utilise the endoscope to look at the last third of the large intestine.
Colonoscopy. This test is similar to sigmoidoscopy, but allows the doctor to look at all of the large intestine using an endoscope. This procedure requires sedation.
Treatment
The most effective treatment for polyps is their removal. Gastroenterologists remove polyps during colonoscopy, and then have the tissue pathologically tested for any presence of cancer. Once a person has had a polyp removed a regular re‑colonoscopic examination is required to reduce the risk of polyp recurrence and cancer formation.