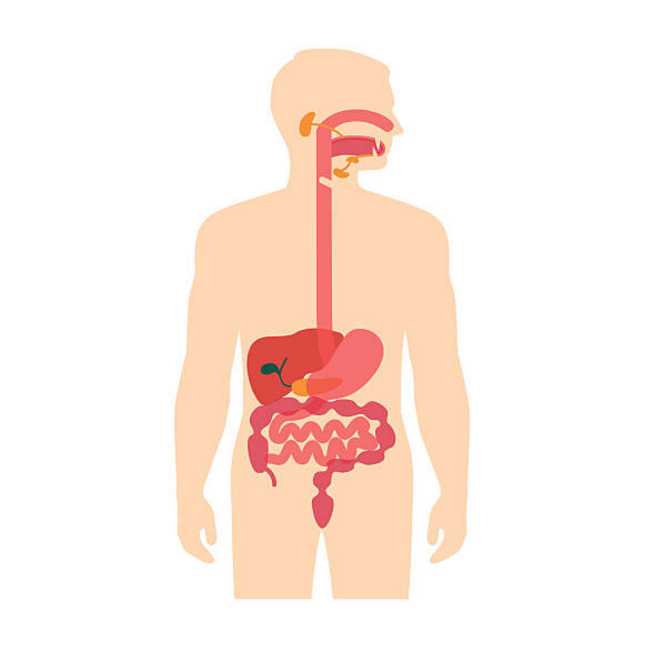
Every surface of the human body is lined with a specialised type of cell that is related to its function. For example, the skin lining our body is different to the mucosa lining the inside of our mouth. This differentiation arises due to the specialised functions of both the linings. Similarly, the lining of the oesophagus whose primary function is to transport ingested food to the stomach is different from the lining of the stomach, which faces an extremely harsh, acidic environment to digest the food consumed.
In Barrett’s oesophagus, there is a change in the lining of the oesophagus. Some of its lining is replaced by a type of tissue similar to that normally found in the intestine. This is called intestinal metaplasia.
Barrett’s oesophagus is closely associated with gastro-oesophageal reflux disease (GORD), in which food and gastric liquids can enter the oesophagus from the stomach. It is presumed that the frequent entry of these liquids into the oesophagus lead to the change of the oesophageal lining.
Barrett’s oesophagus causes no symptoms in itself. However, a small number of people with this condition develop a relatively rare but often deadly type of cancer of the oesophagus called oesophageal adenocarcinoma. This condition was described in the early 1950’s by an Australian surgeon Dr. Norman Rupert Barrett, who noticed that cells lining and extending from the lower oesophagus were secreting red mucus without causing inflammation. He believed these cells formed a tubular stomach in patients who had a short oesophagus however, ten years later he discovered that the mucus-secreting cells were an abnormality of normal cells and led to oesophageal cancer. Hence, this condition is named in honour of Dr. Barrett.
Causes and Symptoms
The exact causes of Barrett’s oesophagus are unknown, but it is thought to be caused in part by the same factors that cause GORD. Although people who do not have heartburn can have Barrett’s oesophagus, it is found about three to five times more often in people with this condition. About 10-20% of people with chronic GORD will develop Barrett’s oesophagus.
The oesophagus is a muscular tube that transports food from the mouth to the stomach. When a person swallows, muscles of the oesophagus relax to accommodate the ingested food at the point of contact but contract above and below this point. Through a sequential and synchronised process, these muscles are able to slowly push segments of food down towards the stomach. This is known as peristalsis. This is the reason food never comes out after we swallow, even if we were lying down or upside down. Going deeper toward the entrance of the stomach, there are strong muscles surrounding the oesophageal tube called sphincters that remain contracted to prevent acids from the stomach from entering the oesophagus. These open only when there is food immediately above to allow food inside the stomach. When people belch to release swallowed air or gas from carbonated beverages, the sphincters relax and small amounts of food or drink may briefly come back up into the oesophagus. This condition is called reflux.
When a person experiences this regularly, especially when not trying to belch, then it is considered a medical problem or disease. The stomach produces acid and enzymes and when this mixture refluxes into the oesophagus frequently, it may produce symptoms. These symptoms, often called acid reflux, are usually described by people as heartburn, indigestion or gas. The symptoms usually consist of a burning sensation below and behind the lower part of the breastbone or sternum. Most people have experienced these symptoms at least once, typically as a result of overeating. Other situations that provoke GORD symptoms include obesity, eating certain types of food and pregnancy. In most people, GORD symptoms may last for only a short time and require no treatment. However, if the symptoms persist and occur regularly then a doctor should be consulted to investigate further. These symptoms, if continuing for some time without relief from ‘over-the-counter’ antacid agents, can contribute to the development of GORD and eventually Barrett’s oesophagus.
The average age of patients diagnosed with Barrett’s oesophagus is 60. In younger ages GORD is much more common than Barrett’s oesophagus. It is about twice as common in men as in women and more common in caucasians than in people of any other ethnicity.
Treatment
Barrett’s oesophagus has no simple cure, besides surgical removal, which is only performed if the patient has a very high risk of developing oesophageal cancer. Treating the associated acid reflux is important and physicians recommend treating GORD with acid-blocking drugs since this can be linked with an improvement in the extent of Barrett’s tissue.
While this is also practiced at the Centre for Digestive Diseases, patients who present with Barrett’s oesophagus may at times undergo treatment with argon plasma coagulation1,2,3 which “burns away” the Barrett’s tissue. This procedure allows the gastroenterologist to remove tissue while performing a panendoscopy. It involves using argon gas and electrical current to result in the very shallow burn of the abnormal tissue without any direct contact. As a result, Barrett’s oesophagus may be treated if it covers only a short area.
A method to remove Barrett’s tissue and therefore, reduce the chance of getting oesophageal cancer, is to freeze off the Barrett’s tissue. The Barrett’s tissue is replaced with normal oesophageal lining providing the patient remains on acid suppressing medication.
1 Pereira-Lima, J.C., Busnello, J.V., Saul, C., Toneloto, E.B., Lopes, C.V., Rynkowski, C.B. & Blaya, C. (2001). High power setting argon plasma coagulation for the eradication of Barrett’s esophagus. The American Journal of Gastroenterology, 96(5): 1662-1663. Doi: 10.1016/S0002-9270(00)00989-8
Link to article: https://www.sciencedirect.com/science/article/abs/pii/S0002927000009898
2 Van Laethem, J.L., Cremer, M., Peny, M.O., Delhaye, M. & Devière, J. (1998). Eradication of Barrett’s mucosa with argon plasma coagulation and acid suppression: immediate and mid term results. Gut, 43: 747-751. Doi: 10.1136/gut.43.6.747
Link to article: https://gut.bmj.com/content/gutjnl/43/6/747.full.pdf
3 Peerally, M.F., Bhandari, P., Ragunath, K., Barr, H., Stokes, C., Haidry, R., Lovat, L., Smart, H., Harrison, R., Smith, K., Morris, T. & de Caestecker, J.S. (2019). Radiofrequency ablation compared with argon plasma coagulation after endoscopic resection of high-grade dysplasia or stage T1 adenocarcinoma in Barrett’s esophagus: a randomized pilot study (BRIDE). Gastrointestinal Endoscopy, 89(4): 680-689. Doi: 10.1016/j.gie.2018.07.031
Link to article: https://www.sciencedirect.com/science/article/abs/pii/S0016510718328980#!